Reimbursement Assistance and Adherence Support
Navigating the complexities of healthcare can be overwhelming, but at AcariaHealth, our dedicated and knowledgeable Reimbursement Teams are here to simplify the process. We ensure you maximize your insurance benefits, help with enrolling in assistance programs, and handle all aspects of your coverage—from billing to direct insurance payments—so you only pay your copay or deductible.
Our network of prescription drug plans, state Medicaid, Medicare, and funding programs helps reduce costs and allows us to provide comprehensive reimbursement support for patients and providers alike. To ensure seamless access to the care you need, our team supports:
- third-party benefits investigations
- prior authorizations
- appeals management
- assistance program enrollment
AcariaHealth also provides personalized refill reminders and ongoing support to ensure medication compliance and the best possible treatment outcomes.
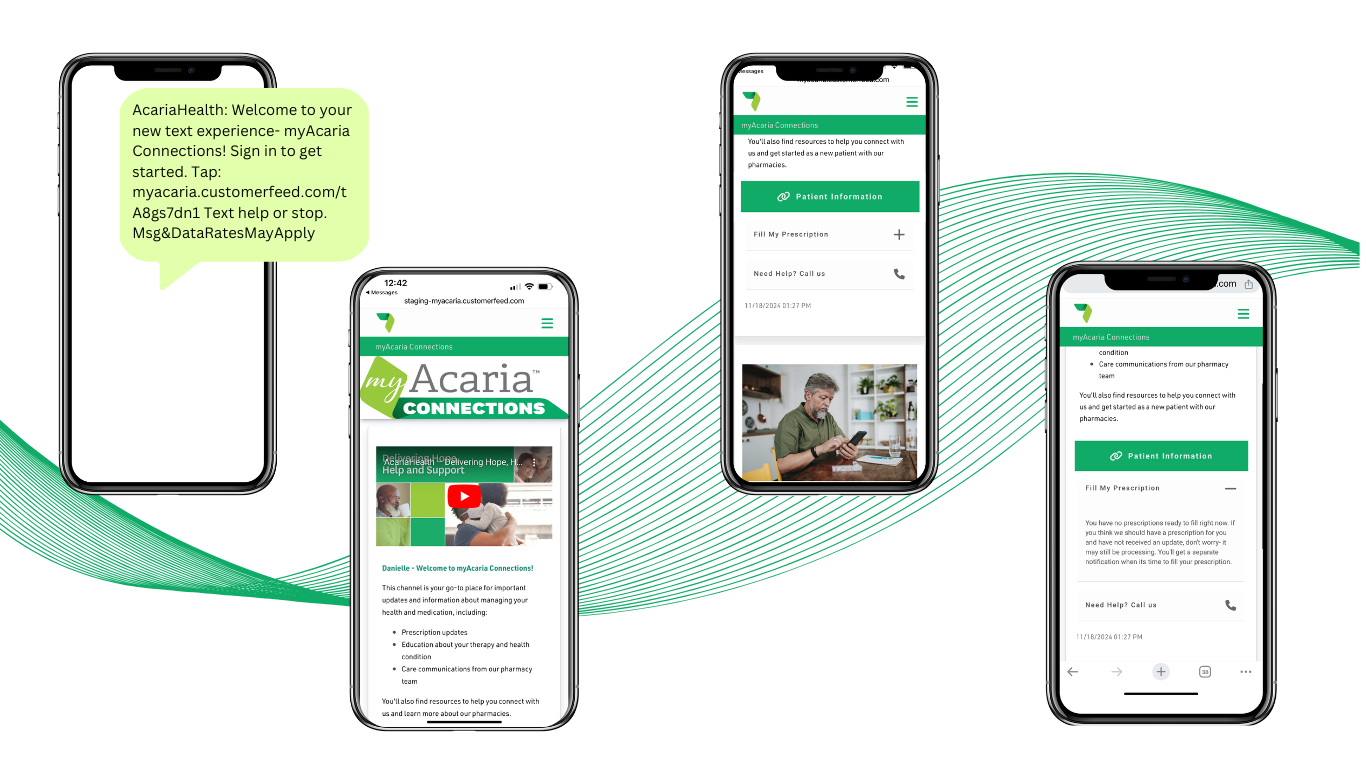
You are encouraged to enroll in our texting service! This convenient and user-friendly digital channel puts full medication management in the palm of your hand.
Intuitive Features
- Order your refill by clicking a link we send you via text
- Get refill reminder and delivery notifications
- Customize your notification preferences
Tailored Resources
- View prescription details
- Read educational materials about your diagnosis
- Watch video instruction of how to administer your medication
Read the Latest
